What is the VH Guide?
The Guide presents advice, scripts, and resources to help navigate conversations about COVID-19 vaccines with hesitant patients. These have been developed with clinicians from across Canada. In the Guide you'll find:
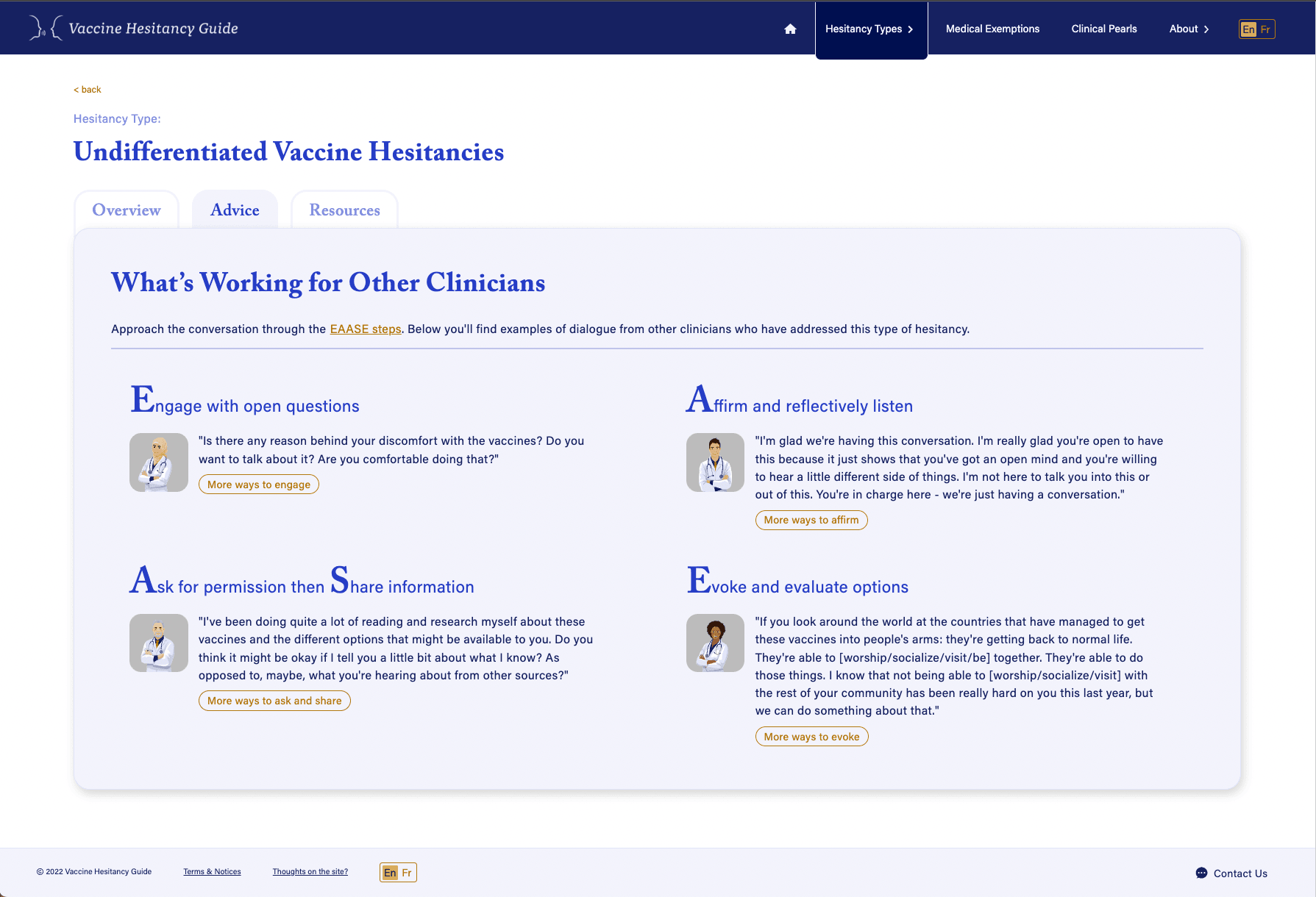
- Clinician-to-clinician adviceon how to counsel patients about their ‘types’‘Type’In this guide, a ‘type’ is a way of grouping together concerns about vaccines or vaccination that share a common psycho-social origin.. Below you’ll find examples of dialogue from other clinicians who have addressed this type of hesitancy.
- Examples of approaches that work for undifferentiated vaccine hesitancy; and
- Aflowsheetfor identifying, differentiating, and addressing common ‘types’‘Type’In this guide, a ‘type’ is a way of grouping together concerns about vaccines or vaccination that share a common psycho-social origin.of vaccine hesitancy
Inside the Guide you will find practical scripts and resources gathered from fellow clinicians that are adapted to each ‘type’ of vaccine hesitancy.
The advice, general principles, and scripts in the guide are grounded in the techniques ofMotivational Interviewing . Motivational Interviewing encourages both the clinician and the patient toidentify positive motivations for vaccination.This happens in the course of open, affirming, conversations about options rather than closed, judgmental, pronouncements of expertise.